Grief is not a contest. Asking what is the hardest grief to deal with usually means you are in the hardest one: the loss that has struck your life. The grieving process is an emotional roller coaster.
Some moments feel manageable, and other moments feel overwhelming. Most people improve as time passes with care, routine and connection. Some people develop enduring symptoms that need focused help.
This guide explains why some griefs feel harder, how specific circumstances influence intensity, what to watch for, and which supports make a difference.
If you want compassionate, Perth-based support while you read, visit our grief counselling page to see session options and book an assessment.
Safety note: If you or someone else is at immediate risk, call 000. For urgent mental health support, contact your GP or a local crisis service.
Why some grief feels harder than others
Grief feels hardest when the loss shatters daily life, social support, or your sense of safety. Severity is shaped by the meaning of the relationship, the way the death happened, and the support around you, not by a universal hierarchy. It makes sense that certain combinations of factors create heavier loads.
Common intensifiers
- How the death happened – A violent death such as a car accident, homicide, or suicide adds shock and threat. These events can imprint sensory memories that trigger intrusive thoughts and a trauma response similar to post traumatic stress disorder.
- Who died and your role – A loved one who was central to your identity changes the shape of your days. The death of a partner, a parent, a sibling, a close friend, or a child can tear holes in routines, finances, parenting, and social life.
- Life context – Financial strain, caregiving load, distance from family members, or cultural stigma can thin out your support groups and services, making it harder to rest and recover.
- History and health – Prior major depression, anxiety, trauma, or medical conditions such as heart disease increase vulnerability to intense symptoms.
- Support quality – Warm, consistent help reduces isolation. Minimising comments, judgment, or silence can increase risk for complicated grief patterns.
The worst grief is the one you are living. That truth does not invalidate anyone else’s grief. It simply honours your personal experience and the work your system is doing to heal.
Is losing a child the hardest type of grief?
The death of a child often brings distinct pressures that many people describe as uniquely disorienting. Parents can experience a profound identity shift, a future abruptly erased, and intense questions about purpose and safety. The mourning process for bereaved parents can surge at milestones such as the first day of school, graduations, birthdays and anniversaries.
If there are grieving children in the home, adults must navigate their own pain while supporting younger people through their grief journey, which can magnify exhaustion.
What can make this grief harder
- Intrusive thoughts about the final moments or counterfactuals such as “if only I had done X.”
- A strong drive to protect surviving siblings that collides with depleted energy.
- Social avoidance from others who do not know what to say, which increases loneliness.
- Guilt and self-blame, even when events were not controllable.
What helps
- Peer programs for child loss, schools that coordinate care plans, and clinicians who understand child bereavement.
- Family sessions to realign roles and language at home. For a practical overview of how counselling can help coordinate care around the table, see Your Guide to Personalised Family Therapy.
Recognising that this is not “normal grief” in complexity does not diminish other losses. It simply names the weight many parents carry so the healing process can be supported well.
What makes grief from suicide loss different?
Suicide loss often blends grief and trauma. Survivors may face shock, stigma, a complex search for “why,” waves of anger and shame, and blame dynamics between family and friends. These pressures are risk factors for developing complicated grief or prolonged grief disorder, especially when people engage in excessive avoidance of places, people and conversations that hold painful reminders.
What helps
- A non-judgemental space to tell the story at your pace.
- Psychoeducation about suicide bereavement so reactions feel understandable rather than “abnormal.”
- Boundaries with social media memorials to reduce re-triggering.
- Survivor-specific support groups and trauma-sensitive counselling.
If there are flashbacks, startle responses, nightmares, or strong avoidance because reminders feel dangerous, seek trauma-informed care. For a stepped path to stabilisation and recovery, read How to Treat PTSD.
Partner loss and the collapse of everyday life
When a partner dies, routines can collapse overnight. If your husband passed or your husband died, the house can go quiet in an instant. Bills, legal forms and logistics can pile up. Even simple tasks like cooking for one can spark intense feelings of emptiness. People tend to judge themselves for not coping faster, then feel guilty for moments of relief. Both reactions are common.
Anchors that help
- Keep a steady sleep window and eat something small by late morning.
- Schedule one practical task before midday to signal capability to your nervous system.
- Invite one trusted person to share dinner once a week to steady social connection.
- Alternate “loss work” with “restoration work” so life holds both pain and recovery in balance.
Disenfranchised grief can intensify pain
Disenfranchised grief is grief that is not socially recognised or supported. Examples include pet loss, the death of an ex-partner, early miscarriage, losses in non-traditional relationships, losses within communities that face stigma, and private caregiving relationships that outsiders did not see. When acknowledgement is missing, isolation increases and so does the risk of prolonged symptoms.
How to re-franchise your grief
- Name the relationship clearly and claim your right to mourn.
- Identify safe listeners rather than trying to educate everyone.
- Create rituals that match the bond, such as a memorial, a letter, or an annual act of service.
Anticipatory grief and terminal illness
Anticipatory grief appears during terminal illness or sustained decline. Caregivers ride a long roller coaster of hope and dread, often while managing work, children and money. Sleep deprivation and physical reactions accumulate. You may feel you must be strong, yet private sadness grows.
Care that protects the future
- Share the load early among family members and friends.
- Ask the treatment team for practical information so decisions feel less chaotic.
- Build micro-routines for food, rest and movement, even if they are brief.
- Allow small goodbyes and honest words now rather than only at the end.
These steps reduce the risk of later clinical depression and improve the mourning process after the death of a loved one.
Grief, trauma and the symptom profile
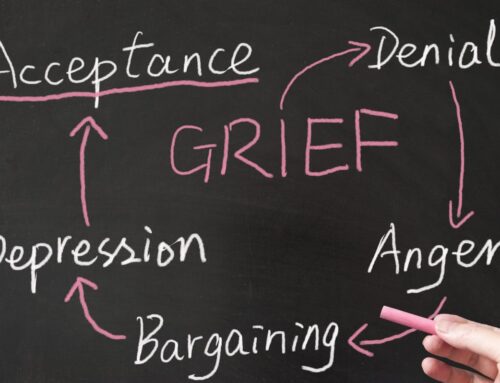
Grief relates to separation and longing. Trauma relates to threat and fear. They can co-occur. Understanding the pattern helps you select care.
- Normal grief: mixed emotions, yearning, sadness, flashes of anger, and gradual reconnection to life. Function returns in steps.
- Prolonged grief disorder: persistent intense sorrow, preoccupation with the deceased, and significant impairment in daily life well beyond culturally expected time frames. This diagnosis replaced persistent complex bereavement disorder in current terminology.
- Post traumatic stress disorder: intrusive images, nightmares, hypervigilance and excessive avoidance because reminders feel dangerous.
- Major depression or clinical depression: global low mood, loss of interest in most activities, feelings of worthlessness or a sense that life is not worth living, often unrelated to specific reminders.
If you are unsure where you sit, speak with a mental health professional. A clear map prevents you from fighting the wrong battle.
Is complicated grief a real diagnosis?
Yes. Prolonged grief disorder is recognised in DSM-5-TR as distinct from typical grief. It involves symptoms such as persistent yearning, identity disruption, disbelief, avoidance of reminders, and marked impairment. People at higher risk include those who faced sudden or violent deaths, had limited social support, or entered bereavement with existing mental health conditions.
Treating complicated grief
- Prolonged grief therapy or complicated grief therapy focuses on telling the story safely, revisiting key memories, restoring roles, and reconnecting with activities and other relationships that sustain you.
- Skills for mood and structure, often drawn from CBT, repair sleep, nutrition and routine while you process the bond.
- When post traumatic stress disorder features are present, trauma stabilisation and gradual exposure sit alongside grief-focused work.
- When major depression overwhelms capacity, GP or psychiatric input on medication may help so therapy can proceed.
To see how skills training reduces avoidance and self-blame, read Cognitive Behavioural Therapy.
Why does grief hit harder at certain times?
Anniversary reactions are common. Dates, seasons, songs, scents and places can trigger a surge. Many people notice stronger waves during birthdays, death dates, holidays and family gatherings. These waves are a normal part of the grieving process, not a setback.
Planning steps
- Keep the day lighter if you can and invite a support person to check in.
- Choose a personal ritual that provides comfort, such as lighting a candle, visiting a meaningful place or sharing a favourite meal.
- Name the wave out loud so your system understands what is happening.
- If your body stays on high alert, read Somatic Psychotherapy for body-based tools that calm arousal.
Can grief resurface years later?
Yes. Grief often reappears around life transitions and anniversaries. A new child, moving house, retirement, ill health, or a major achievement can pull forward memories. A returning wave does not mean failure to cope. It means the bond still matters.
How to check the wave
- Sleep: can you get a few nights of reasonable rest each week.
- Function: can you handle essential tasks even if you pause others.
- Connection: can you reach one safe person or attend a group.
If weeks pass and you feel stuck, therapy can help you re-engage with life while honouring the bond. For a plain-language overview of what psychotherapy offers, see What Does Psychotherapy Do.
Why do some people never recover from loss?
Most people do adapt, but recovery looks like living with grief, not erasing it. When people say someone never recovered, they often mean ongoing impairment or a life narrowed around the loss. Factors that maintain suffering include isolation, excessive avoidance of reminders, untreated trauma, and untreated depression.
When to widen support
- You cannot return to core daily activities or self-care for many weeks.
- You rely on alcohol or drugs to numb painful emotions.
- Sleep and appetite remain severely disrupted.
- You experience a persistent sense that life is not worth living.
Layer supports: peer groups, routines, therapy and a medical review to screen for major depression or other conditions. For treatment options, read How to Treat Depression.
What does healthy grieving look like?
Healthy grieving shows sadness alongside growing capacity for daily life, connection and meaning. Markers include basic routines that keep going, moments of warmth or purpose, and the ability to remember without total shutdown. Pace is personal and shaped by culture and family rituals. There is no single correct timeline.
Everyday practices that help
- Keep a regular sleep window and morning light.
- Eat small, regular meals and drink water even when appetite dips.
- Take short walks or gentle stretches to move stress through the body.
- Use values-based rituals such as letters, memorials or service.
- Share stories about the loved one at a pace that feels right.
- Ask for practical help and set kind boundaries when you need rest.
To understand how talking therapies can support different stages of the journey, see Psychotherapy.
Physical reactions that make grief feel overwhelming
Grief lives in the body as well as in thoughts and feelings. Physical reactions can include chest tightness, headaches, stomach upset, muscle tension, dizziness after crying, and a shaky sense of balance when approaching certain places. These symptoms are common. When severe, new or worsening, see your GP to rule out medical causes. If you have a history of heart disease or other health conditions, keep your routine care in view during bereavement.
Gentle regulation for the body
- Slow breathing, 4 seconds in and 6 seconds out, for a few minutes.
- Open a window or step outside for sunlight and air.
- Warm showers, weighted blankets or comfortable clothes that cue safety.
- Limit caffeine late in the day and reduce alcohol, which can amplify anxiety and low mood.
Grieving children and teens
Children grieve in bursts. Play may return quickly, then big emotions arrive again at bedtime or school drop-off. Teens often oscillate between independence and closeness, between silence and intense conversation.
How to help
- Use clear, concrete language and honest answers. Avoid euphemisms that create confusion.
- Keep daily routines as steady as possible. Predictability is calming.
- Invite questions over time and accept that the same question may return at new developmental stages.
- Offer choices for participation in rituals and remembrance.
- Seek help early if school collapses, withdrawal persists, or risk-taking rises.
Evidence-based paths for treating complicated grief
When symptoms remain strong for months, or life does not restart, you may be meeting criteria for prolonged grief disorder. The older term persistent complex bereavement disorder is still used in some places. The goal of care is not to erase grief, but to help you live your own life while honouring the bond.
Core elements
- Telling the story safely. Structured sessions that allow you to approach the memory without flooding.
- Restoring roles. Stepwise re-entry into tasks, work or study so life regains rhythm.
- Reconnecting with values. Activities and relationships that fit who you are now.
- Reducing avoidance. Gentle, graded visits to places and situations that matter, so your world can widen again.
- Addressing beliefs. Shifting self-blame, catastrophic thinking and rigid rules that keep suffering in place.
- Checking comorbidities. Screening for post traumatic stress disorder, clinical depression, sleep disorders or substance use so nothing essential is missed.
These components are often combined in a tailored plan that respects culture, language, spirituality and community.
Practical ways to soften hard grief
- Steady your day. Keep a simple sleep window, morning light and one small task before midday.
- Name the wave. Say what the trigger is and what you need, such as space, company, or help with a chore.
- Choose connection. Ask one trusted person for a check-in on tender dates and consider a peer group that understands your type of loss.
- Use rituals. Light a candle, visit a meaningful place, cook a favourite recipe, or create a small memorial at home.
- Protect your body. Eat regular meals, hydrate, and reduce alcohol or other substances that can amplify anxiety or low mood.
- Track patterns. Note what helps and what hurts. Refresh your plan as seasons change.
- Seek timely care. If symptoms remain intense or you cannot function, ask for an assessment and a clear plan with a mental health professional.
Final thought
If you are searching for what is the hardest grief to deal with, you may already be carrying it. The most important thing is not to judge your progress by anyone else’s timeline. Your relationship was unique. Your emotional journey will be unique as well. Grief can be painful, chaotic, and strange. It can also open moments of tenderness, gratitude and connection that remind you why the bond mattered. With routine, connection, and the right help when needed, the healing continues. The love you carry does not end because the person died. You are allowed to grieve, to live, and to let both truths co-exist as you move forward.
Related Posts
Fees And Rebates
We offer cost-effective solutions that can fit within your budget. The insights and skills acquired in therapy can continue to positively impact mental and emotional health long after the therapy sessions have ended, making it a truly worthwhile investment in yourself.