Grief is a natural response to the death of a loved one, and it rarely unfolds in a straight, predictable line. When people ask, “What are the 7 stages of grief after a death?”, they are usually looking for a simple way to understand difficult feelings. The seven stages most commonly listed are shock, denial, anger, bargaining, depression, testing or upward turn, and acceptance. Treat these stages as a teaching tool, not a rulebook. Not everyone will experience every stage, and the grieving process does not follow a particular order. Feelings can overlap, repeat, or arrive in waves as you adjust to a new reality. Use the model to name what is happening, then focus on gentle coping strategies that support sleep, appetite, movement, and connection.
If intense sadness, anxiety, or functional problems persist for weeks to months, a mental health or grief counselling professional can help you assess for conditions like prolonged grief disorder and guide the healing process.
What do the 7 stages of grief mean?
The seven stages describe common reactions after a death, not a strict checklist every person must follow. These stages of grief are teaching tools to help with understanding grief, to normalise difficult feelings, and to offer language when words are hard. The grieving process is rarely a straight line. It moves in waves, and stages can repeat, blend, or appear out of any particular order. There is no right or wrong way to grieve, and not everyone will relate to all seven stages.
What are the 7 stages in plain language?
Use these as signposts, not steps you must tick off. Stages can overlap, repeat, or arrive in any order.
1. Shock
A jolt to your sense of reality. Numbness, disbelief, and autopilot behaviour are common. You might keep making tea for a loved one who has died, or drive to their job out of habit. Physical symptoms can include shaky hands, a tight chest, or a frozen feeling. Sleep may be disrupted for days or weeks.
2. Denial
A protective pause. You may avoid reminders, keep their clothes where they were, or speak as if the family member will walk back in. Denial is not a mistake, it buys time for the nervous system to adjust to the reality of the death and dying.
3. Anger
It is common to feel anger, at events, people, systems, yourself, or even a higher power. You might resent red tape, a slow ambulance, an argument you had, or the sheer wrong ness that this could happen. Anger is energy, and with safe outlets it can fuel advocacy, ritual, or care for others.
4. Bargaining
The classic bargaining stage. You may think, “If only I had insisted on another test,” or “If I do everything right, maybe the pain will ease.” Bargaining tries to restore control when life feels unmanageable. It is a normal, natural response to loss.
5. Depression
This is the heavy, quiet valley, sadness, low energy, loss of interest, withdrawal, foggy concentration. You might feel helpless, feel guilty, or wonder whether life can hold meaning again. Sleep, appetite, and motivation often fluctuate. If this persists with a global loss of interest, it may overlap with clinical depression. Consider the guidance below on when to seek help.
6. Testing
Sometimes called the upward turn. You try small experiments that reconnect you with people and place, replying to two texts, eating breakfast at a table, walking with a friend, or returning to one support group. Testing is tentative progress, not the final stage.
7. Acceptance
Acceptance means recognising the loss and finding ways to carry love and emotions together. It is not “being over it”. You make room to cope, handling bills, resuming work or study, speaking the person’s name without total collapse, and allowing warmth, purpose, and memory to co exist.
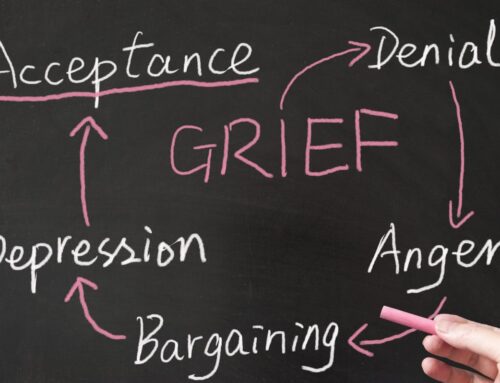
Who created the 7 stages of grief model?
There is no single, definitive medical source for “the seven stages of grief”. The idea grew out of public education and earlier frameworks. The best known precursor is the Kübler Ross model, proposed by Kübler Ross, a Swiss American psychiatrist, who described the five stages of grief in people who were terminally ill individuals facing their own dying.
Those five are denial anger bargaining depression and acceptance. Educators later adapted and expanded these lists for bereavement by adding “shock” and “testing”. Treat stages as helpful language, not a diagnosis.
Are the 7 stages of grief always experienced in order?
No. People grieve in unique sequences. Some people grieve by circling two or three stages for months, others notice brief touches of several grief stages in a single day. Order varies with your history, the relationship to the person, community and cultural supports, and practical realities like insurance coverage, leave from work, or the demands of caring for others during a terminal illness. Track your patterns, sleep, appetite, connection, daily tasks, rather than chasing a perfect sequence.
Is the 7 stages of grief model accurate?
Useful, with limits.
Strengths: the model names difficult feelings, creates a shared vocabulary for families, and reassures people that emotions like anger, guilt, and numbness are common.
Limits: it can oversimplify and make you worry you are doing grief “wrong” if your experience does not match. Use stages as a map to start conversations. When you want a clearer sense of how therapy supports the healing process beyond stages, read What Does Psychotherapy Do.
What is the difference between the 5 and 7 stages of grief?
The five stages are denial, anger, bargaining, depression, and acceptance. Seven stage versions add shock at the beginning and testing as people try small steps back into life. Both are frameworks that organise experience. Choose whichever description helps you name what you experience feelings of today. For broader options across talking therapies during bereavement, see Psychotherapy.
Can you skip stages of grief?
Yes. You can skip, repeat, or blend stages and still grieve healthily. A parent caring for a child through a terminal illness, for example, may live in testing and depression at once, with bursts of anger after medical updates. Others never relate to bargaining but strongly feel shock and numbness. Notice what helps, not where you are on a chart.
How long does each stage of grief last?
There is no set time. Duration depends on the bond with the person, the circumstances of the death and dying, your health, and your support. Consider extra help if severe distress and functional impairment continue for weeks to months, if you have risk thoughts, or if anxiety, sleep and appetite remain badly disrupted. A simple fortnightly check helps, one sleep goal, one meal goal, one connection, and one task. If you need help finding a practitioner who fits, see Counselling Services Near Me How to Find the Best Counsellor.
Do children go through the 7 stages of grief?
Children grieve differently by age. Young children may show their emotions in behaviour, clinginess, irritability, tummy aches, more than words. Teens may move between independence and sudden closeness. Use clear, concrete language, stable routines, and repeat invitations to talk. Offer choices about participation in farewells and memorials so they can cope at a safe pace. For guidance that brings everyone to the same table, read Your Guide to Personalised Family Therapy.
What stage of grief is anger?
Anger can appear early, late, or in waves. It is a universal experience in grief, and it does not mean you are doing something wrong. Safe outlets include brisk walks, punching pillows, writing unsent letters, or channelling energy into advocacy or ritual. Keep boundaries if anger risks harm to you or others, and name its target, the illness, the system, your decision, to reduce shame and blame. Skills that steady thoughts and behaviour can help, see Cognitive Behavioural Therapy for Anger Management.
Is it normal to feel numb after someone dies?
Yes. Numbness and disconnection are common in early grief and during later spikes. They are short term protection responses. Feeling often returns in brief bursts, then retreats again. Gentle regulation helps, regular meals, light movement, slow breathing, and morning daylight. If numbness persists with functional decline or strong anxiety, talk with your GP. For comparison points, read What Are the Signs of Anxiety.
When do stages become something else, like prolonged grief disorder?
Most people find capacity returns, bit by bit, as they test routines, ask for support, and discover meaning. A minority develop enduring symptoms. Prolonged grief disorder, sometimes called complicated grief, involves persistent yearning or preoccupation with the deceased and marked impairment for many months beyond cultural expectations. If depression becomes global, no interest in anything, low energy, hopelessness, or if you cannot function day to day, speak with a mental health professional or mental health expert. Targeted support helps distinguish grief from conditions like major depression and guides the healing process.
Red flags to discuss with a clinician
- Severe, lasting inability to work, study, or care for yourself
- Reliance on alcohol or drugs to sleep or numb
- Persistent beliefs that life is not worth living
- Extreme isolation or guilt you cannot shift
How to use the stages kindly, and practically
- Treat stages as descriptions, not tasks. They are a shared vocabulary for feelings, not a scorecard.
- Track function, not perfection. Check sleep, meals, movement, and one connection rather than “Which stage am I in”.
- Expect mixes. You can accept the reality of the death and still feel surges of anger.
- Keep supports concrete. Ask, “Please text before visiting”, or “Could you drive me to the GP”.
- Hold space for meaning. Some people connect with a higher power, others honour values through service, art, or nature. Either path can help the healing process.
- Review practicalities. Time off, finances, superannuation, and insurance coverage can affect stress and access to care. Practical help is emotional help.
Bottom line
The 7 stages of grief offer a shared language for a human experience that is bigger than any list. Use them to name what is happening, then return to what sustains you, sleep, food, movement, conversation, ritual, and timely help. If the path feels stuck or the load is too heavy, a mental health professional can help you build a plan that respects your story and restores the parts of life that matter most.
Related Posts
Fees And Rebates
We offer cost-effective solutions that can fit within your budget. The insights and skills acquired in therapy can continue to positively impact mental and emotional health long after the therapy sessions have ended, making it a truly worthwhile investment in yourself.